Female Reproductive System Organs, Functions & Hormones: A Complete Guide with Real-World Relevance
Lesson Overview
The female reproductive system is essential for reproduction, growth, and overall health. This lesson will help you understand its organs, functions, and the hormones involved in regulating various processes. Understanding this system is crucial for learning about fertility, health, and the biological changes that occur throughout a woman's life.
What Is the Female Reproductive System?
The female reproductive system is a complex network of organs responsible for reproduction, hormone production, and maintaining overall reproductive health. It includes both internal and external structures that work together to enable menstruation, fertilization, pregnancy, and childbirth.
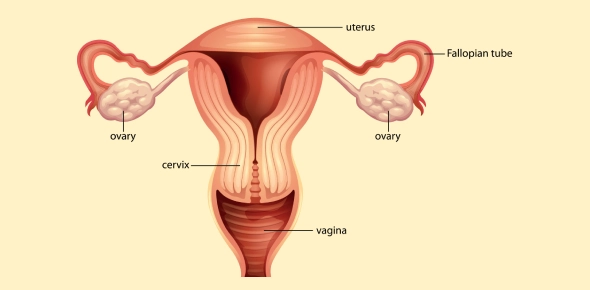
Fig: Female Reproductive System Diagram
Female Anatomy: Major Organs and Their Functions
The female reproductive system consists of both internal and external structures, each playing a vital role in functions such as egg production, fertilization, menstruation, pregnancy, and childbirth.
External Female Anatomy
The external reproductive organs are collectively known as the vulva and serve as the body's first barrier against infections while also playing a role in sexual pleasure.
1. Vulva
The vulva refers to all the external parts of the female anatomy that protect the internal organs and aid in reproductive and sexual functions. It includes:
- Labia Majora – The outer folds of skin that enclose and protect the external reproductive organs. These structures contain sweat and oil glands and may have hair after puberty.
- Labia Minora – The inner, smaller folds of skin located inside the labia majora, surrounding the vaginal and urethral openings. They provide protection and contain many nerve endings, enhancing sensitivity.
- Clitoris – A highly sensitive, small organ located at the upper part of the labia minora. It plays a crucial role in pleasure due to its rich nerve supply.
- Vaginal Opening – The entrance to the vagina, located below the urethral opening. It allows for menstrual flow, intercourse, and childbirth.
Fig: Parts of the Vaginal System
Internal Female Anatomy
The internal reproductive organs are responsible for egg production, fertilization, and pregnancy. They include the ovaries, fallopian tubes, uterus, cervix, and vagina-all working together to support reproductive functions.
2. Ovaries
The ovaries are two small, oval-shaped glands located on either side of the uterus. They are essential for:
- Egg Production (Oogenesis) – The ovaries store thousands of immature eggs and release one mature egg each month during ovulation.
- Hormone Production – The ovaries produce estrogen and progesterone, which regulate the female reproductive system function, control the menstrual cycle, and support pregnancy.
Fig: Diagram of Human Female Ovary
3. Fallopian Tubes
The fallopian tubes are thin tubes that connect the ovaries to the uterus. They play a vital role in:
- Transporting the Egg – After ovulation, the egg is released into the fallopian tube, where tiny hair-like structures (cilia) move toward the uterus.
- Site of Fertilization – If sperm is present, fertilization typically occurs in the fallopian tube before the fertilized egg moves to the uterus for implantation.
Fig: A diagram of the female reproductive system shows the fallopian tube, a fertilized egg traveling toward the uterus, the ovary releasing an egg, and a developing fetus inside the womb.
4. Uterus
The uterus, also known as the womb, is a muscular, pear-shaped organ responsible for supporting pregnancy. Its main functions include:
- Menstruation – If no fertilization occurs, the inner lining (endometrium) sheds, leading to menstrual bleeding.
- Implantation and Pregnancy – If an egg is fertilized, it implants in the uterus, where it grows and develops into a fetus.
- Labor and Childbirth – The uterine muscles contract during labor to deliver the baby.
Fig: A diagram depicting the uterus with a developing baby inside, shows the structure of the womb and its role in pregnancy.
5. Cervix
The cervix is the lower, narrow portion of the uterus that connects to the vagina. It has several critical roles:
- Menstrual Flow – The cervix allows blood from the uterus to exit the body during menstruation.
- Sperm Passage – During ovulation, the cervix produces mucus that helps sperm travel into the uterus for fertilization.
- Protection During Pregnancy – The cervix remains tightly closed during pregnancy to protect the fetus and only opens during labor.
Fig: A diagram of cervix thinning and widening during labor
6. Vagina
The vagina is a muscular, flexible canal that connects the cervix to the external body. It serves multiple functions, including:
- Sexual Intercourse – The vagina facilitates penetration during intercourse and expands to accommodate arousal and childbirth.
- Menstrual Flow Exit – Blood exits the body through the vagina during menstruation.
- Birth Canal – The vagina stretches significantly during childbirth to allow the baby to pass through.
All components of the female reproductive system work together in harmony to ensure proper reproductive health. Their key interactions include:
- Ovaries release an egg (ovulation), which travels through the fallopian tubes.
- If fertilization occurs, the fertilized egg implants in the uterus and develops into a fetus.
- If fertilization does not occur, the uterus sheds its lining (menstruation).
- The cervix controls access between the uterus and the vagina, regulating sperm entry and protecting the fetus during pregnancy.
Understanding women's reproductive organs is crucial for maintaining reproductive health and recognizing potential medical conditions. Each organ plays an essential role in the female reproductive system function.
Take This Quiz :
Functions of the Female Reproductive System
The female reproductive system is designed to support various biological processes, including menstruation, ovulation, fertilization, pregnancy, and childbirth. Each organ within the system has a specific function, but together, they ensure the reproductive cycle runs smoothly.
1. Egg Production and Ovulation
One of the primary female reproductive system functions is oogenesis, or the production of eggs (ova). This process occurs in the ovaries, where thousands of immature eggs are stored. Once a month, one egg matures and is released in a process called ovulation.
- Ovaries – Contain follicles that develop into mature eggs.
- Ovulation – The release of an egg from the ovary, typically occurring around the 14th day of a 28-day cycle.
2. Hormone Production and Regulation
The female reproductive system produces essential hormones that control reproductive functions and influence secondary sexual characteristics like breast development and menstrual cycles.
- Estrogen – Responsible for the development of female secondary sexual characteristics and regulating the menstrual cycle.
- Progesterone – Prepares the uterus for pregnancy by thickening the uterine lining.
- Follicle-Stimulating Hormone (FSH) & Luteinizing Hormone (LH) – Regulate ovulation and the menstrual cycle.
3. Menstruation: The Monthly Cycle
If fertilization does not occur, the female reproductive system function includes menstruation, where the uterus sheds its inner lining. This cycle repeats every 28 days on average and consists of four phases:
- Menstrual Phase (Days 1-5) – The uterine lining sheds, leading to menstrual bleeding.
- Follicular Phase (Days 1-13) – The body prepares for ovulation, and estrogen levels rise.
- Ovulation (Day 14) – The egg is released from the ovary.
- Luteal Phase (Days 15-28) – If fertilization doesn't happen, progesterone levels drop, triggering menstruation.
4. Fertilization and Pregnancy Support
A major female reproductive system function is facilitating fertilization and pregnancy. Once an egg is released, it travels through the fallopian tube, where it may meet sperm. If fertilization occurs, the zygote moves to the uterus for implantation.
- Fallopian Tubes – Serve as the meeting place for sperm and egg.
- Uterus – Supports the fertilized egg and nurtures fetal development.
- Placenta – Forms to provide oxygen and nutrients to the growing fetus.
5. Childbirth: The Role of the Uterus and Cervix
Toward the end of pregnancy, the uterus prepares for labor by contracting and pushing the baby through the cervix and vagina.
- Dilation of the Cervix – The cervix gradually opens to allow for birth.
- Uterine Contractions – The muscular walls of the uterus contract to push the baby out.
- Delivery of the Placenta – The placenta is expelled after childbirth.
6. Lactation: The Post-Pregnancy Function
After childbirth, the female reproductive system function extends to breastfeeding. The hormone prolactin stimulates milk production in the mammary glands, and oxytocin helps with milk ejection.
The Menstrual Cycle and Ovulation
The menstrual cycle and ovulation are essential processes that prepare the body for potential pregnancy. These cycles are controlled by hormonal changes that regulate the release of an egg and the preparation of the uterus for implantation. If fertilization does not occur, the body sheds the uterine lining, leading to menstruation.
The average cycle lasts about 28 days, but it can vary between 21 to 35 days depending on individual physiology. It consists of four main phases:
- Menstrual Phase (Days 1-5): Shedding of the uterine lining (period).
- Follicular Phase (Days 1-13): Egg development and preparation for ovulation.
- Ovulation Phase (Day 14): Release of a mature egg from the ovary.
- Luteal Phase (Days 15-28): Uterus prepares for implantation or resets for a new cycle.
Fig: Menstrual Cycle Diagram
Take This Quiz :
Hormones and Their Role in Female Reproduction
The primary hormones involved in the female reproductive system function are:
- Estrogen – This regulates the menstrual cycle and supports reproductive health.
- Progesterone – This prepares and maintains the uterus for pregnancy.
- Follicle-Stimulating Hormone (FSH) – This stimulates egg growth in the ovaries.
- Luteinizing Hormone (LH) – This triggers ovulation and corpus luteum formation.
- Gonadotropin-Releasing Hormone (GnRH) – This controls FSH and LH production.
- Human Chorionic Gonadotropin (hCG) – This supports early pregnancy.
- Prolactin – This affects milk production after childbirth.
- Oxytocin – This triggers contractions during labor and milk ejection.
Importance of the Female Reproductive System
The female reproductive system is essential for several key reasons:
- Overall Health: The proper functioning of the female reproductive system is linked to overall health and well-being. Issues with the system can sometimes indicate or contribute to other health problems.
- Reproduction: Its primary function is to enable sexual reproduction, allowing for the creation of offspring. This involves the production of eggs, fertilization by sperm, and the nurturing of a developing embryo and fetus.
- Hormone Production: The ovaries, part of the female reproductive system, produce crucial hormones like estrogen and progesterone. These hormones regulate the menstrual cycle, play a role in sexual development, and influence other aspects of health, including bone density and mood.
- Childbearing: The uterus provides a safe and nurturing environment for a developing fetus during pregnancy. The system also facilitates childbirth.
Rate this lesson:
 Back to top
Back to top
(234).jpg)