Liver Lesson: Structure, Anatomy, Functions
Lesson Overview
- What Is the Liver?
- What Is the Structure of the Liver?
- What Is the Liver's Role in Digestion?
- What Is the Liver Detoxification Process?
- What Is the Role of Liver Enzymes?
- How Does the Liver Produce Bile and What Is Its Function?
- What Are Common Liver Diseases?
- How Can We Maintain Good Liver Health?
- Conclusion
The liver is one of the largest and most vital organs in the human body, playing a central role in digestion, metabolism, detoxification, and nutrient storage. Located in the upper right side of the abdomen, the liver works continuously to filter blood, process nutrients, and remove harmful substances. This lesson explores the structure and anatomy of the liver, including its lobes and internal arrangement, and outlines its key functions that support overall health.
What Is the Liver?
The liver is a large, reddish-brown organ located in the upper right side of the abdomen, just below the diaphragm and above the stomach. It is the largest internal organ and the heaviest gland in the human body, weighing about 1.4 to 1.6 kilograms in adults. The liver performs over 500 essential functions, making it crucial for maintaining life and health.
Key Characteristics of the Liver:
- Divided into two main lobes: right and left
- Receives blood from two sources: the hepatic artery (oxygen-rich) and the portal vein (nutrient-rich from the intestines)
- Enclosed in a thin, fibrous capsule and protected by the lower ribs
- Made up of functional units called lobules, which contain hepatocytes (liver cells)
What Is the Structure of the Liver?
The liver has a complex yet highly organized structure that supports its wide range of functions. It is composed of lobes, lobules, blood vessels, bile ducts, and specialized cells. This structure allows the liver to filter blood, produce bile, store nutrients, and detoxify harmful substances efficiently.
External Structure
1. Lobes of the Liver
- The liver is divided into two main lobes:
- Right lobe: larger
- Left lobe: smaller
- It also includes two smaller lobes (visible internally):
- Caudate lobe
- Quadrate lobe
- The lobes are separated by the falciform ligament, which also anchors the liver to the abdominal wall.
Internal Structure
2. Lobules (Functional Units)
- The liver is made up of microscopic units called lobules
- Each lobule is shaped like a hexagon and consists of hepatocytes (liver cells) arranged in plates
- In the center of each lobule is a central vein that collects filtered blood
- At the corners of the lobule are portal triads, which include:
- A branch of the hepatic artery (brings oxygen)
- A branch of the portal vein (brings nutrients from intestines)
- A bile duct (carries bile to the gallbladder)
3. Blood Supply
- Dual blood supply:
- Hepatic artery delivers oxygen-rich blood
- Portal vein delivers nutrient-rich blood from the gastrointestinal tract
- Blood flows through sinusoids, where it is filtered by hepatocytes before draining into the central vein
4. Bile Canaliculi and Ducts
- Bile canaliculi are small channels between hepatocytes that collect bile
- Bile flows from canaliculi → bile ducts → hepatic duct → gallbladder or small intestine
Protective Covering
- The liver is covered by a thin, tough membrane called Glisson's capsule
- It also has a peritoneal covering for protection and support

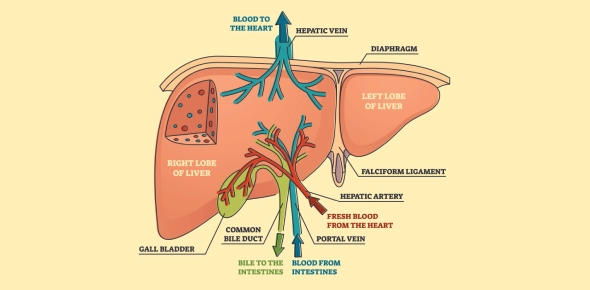
Fig: Labeled Diagram of the Anatomy of the Liver
Take These Quizzes
What Is the Liver's Role in Digestion?
The liver plays a crucial role in digestion by producing bile, a digestive fluid essential for breaking down fats in the small intestine. Although the liver doesn't digest food directly, it supports and regulates many processes that make digestion efficient and effective.
Key Digestive Functions of the Liver
1. Bile Production
- The liver produces bile, which contains bile salts, water, cholesterol, and pigments
- Bile emulsifies fats, breaking them into small droplets for easier digestion by enzymes like lipase
- Bile is stored in the gallbladder and released into the duodenum when fatty food enters the small intestine
2. Processing Nutrients
- After absorption in the small intestine, nutrient-rich blood travels to the liver via the portal vein
- The liver converts, stores, or distributes nutrients as needed:
- Glucose → stored as glycogen
- Amino acids → used for protein synthesis or converted to energy
- Fats → metabolized or stored
3. Detoxification
- The liver filters and neutralizes toxins, including alcohol, drugs, and metabolic waste
- Converts harmful substances into less toxic compounds for excretion
4. Synthesis of Plasma Proteins
- Produces albumin, which maintains blood volume and pressure
- Synthesizes clotting factors, which help in wound healing and prevent bleeding
5. Storage of Vitamins and Minerals
- Stores fat-soluble vitamins (A, D, E, K) and minerals like iron and copper
- Releases them into the bloodstream when required
What Is the Liver Detoxification Process?
The liver detoxification process refers to the liver's ability to neutralize, break down, and eliminate harmful substances from the blood. These substances include toxins, drugs, alcohol, metabolic waste, and byproducts of digestion. Detoxification is essential for protecting the body from damage and maintaining internal balance.
Key Phases of Liver Detoxification
Phase I: Modification (Oxidation, Reduction, Hydrolysis)
- Involves enzymes, mainly the cytochrome P450 system
- These enzymes convert toxins into intermediate compounds-often more water-soluble, but sometimes more reactive
- Examples of substances processed: alcohol, caffeine, medications, environmental toxins
Phase II: Conjugation
- Phase I byproducts are joined with other molecules to neutralize and prepare them for excretion
- Uses processes like glucuronidation, sulfation, acetylation, and methylation
- Converts fat-soluble toxins into water-soluble forms
- These compounds are then excreted via bile (feces) or urine
Supporting Elements of Detoxification
| Component | Role |
|---|---|
| Enzymes | Facilitate chemical reactions in both phases |
| Antioxidants | Neutralize free radicals produced in Phase I |
| Amino Acids | Provide building blocks for conjugation |
| Water | Helps flush out water-soluble toxins through urine |
| Bile | Carries fat-soluble toxins into the intestines for elimination |
Organs Involved in Final Elimination
- Kidneys: Filter and excrete water-soluble waste in urine
- Intestines: Eliminate fat-soluble waste via bile and feces
- Skin and lungs: Secondary pathways through sweat and breath
Why Liver Detoxification Is Important
- Protects organs from toxin damage
- Maintains chemical balance in the blood
- Helps metabolize hormones, medications, and environmental pollutants
- Prevents the buildup of free radicals that contribute to aging and disease
What Is the Role of Liver Enzymes?
Liver enzymes are proteins produced by liver cells that help regulate a wide range of chemical reactions necessary for digestion, detoxification, metabolism, and other vital processes. These enzymes also serve as important biomarkers in medical tests to assess liver function and detect liver damage or disease.
Key Roles of Liver Enzymes
1. Detoxification
- Enzymes such as those in the cytochrome P450 system break down toxins, drugs, and alcohol
- Convert harmful substances into less toxic forms for excretion through urine or bile
- Play a central role in Phase I and Phase II detoxification processes
2. Metabolism of Nutrients
- Help metabolize carbohydrates, proteins, and fats
- Convert glucose into glycogen for storage and back again when energy is needed
- Assist in the synthesis and breakdown of amino acids and cholesterol
3. Bile Production Support
- Enzymes aid in the production and secretion of bile acids, which are crucial for fat digestion and absorption
- Also help recycle bile components efficiently
4. Protein Synthesis
- Assist in producing albumin, the main blood protein that maintains fluid balance
- Aid in forming clotting factors, which help in blood coagulation
5. Regulation of Hormones and Vitamins
- Metabolize and regulate hormones such as estrogen, insulin, and cortisol
- Help activate and store fat-soluble vitamins like A, D, E, and K
Common Liver Enzymes and Their Diagnostic Use
| Enzyme | Full Name | Function | Diagnostic Significance |
|---|---|---|---|
| ALT | Alanine Aminotransferase | Breaks down amino acids | Elevated in liver cell damage |
| AST | Aspartate Aminotransferase | Converts amino acids and supports energy | Elevated in liver or muscle damage |
| ALP | Alkaline Phosphatase | Involved in bile flow and bone health | Elevated in bile duct or bone disorders |
| GGT | Gamma-Glutamyl Transferase | Supports bile transport and detox | Elevated in alcohol-related liver disease |
Why Liver Enzymes Matter
- Essential for metabolic and detox pathways
- Help maintain chemical balance in the body
- Serve as indicators of liver health in routine blood tests
- Guide diagnosis and treatment of liver conditions such as hepatitis, fatty liver, and cirrhosis
How Does the Liver Produce Bile and What Is Its Function?
The liver produces bile, a yellow-green fluid essential for digesting and absorbing fats. Bile is synthesized by hepatocytes (liver cells) and plays a crucial role in the digestive process, particularly in the small intestine. Once produced, bile is either sent directly to the duodenum or stored temporarily in the gallbladder.
How the Liver Produces Bile
- Secretion by Hepatocytes
- Hepatocytes produce bile continuously from cholesterol, water, bile salts, pigments (like bilirubin), and electrolytes
- Bile acids are synthesized from cholesterol and are the primary active components of bile
- Flow Through Canaliculi and Ducts
- Bile flows from hepatocytes into tiny channels called bile canaliculi
- From there, it moves into larger bile ducts, eventually reaching the common hepatic duct
- Storage or Release
- If digestion is not occurring, bile flows into the gallbladder via the cystic duct, where it is stored and concentrated
- During digestion (especially after eating fatty foods), bile is released into the duodenum through the common bile duct
Functions of Bile
1. Emulsification of Fats
- Bile salts break large fat globules into smaller droplets, increasing the surface area for enzymes (lipases) to act
- This emulsification is essential for efficient fat digestion
2. Absorption of Fat-Soluble Nutrients
- Bile helps in the absorption of fat-soluble vitamins A, D, E, and K
- It also aids in the absorption of cholesterol and other lipids
3. Excretion of Waste Products
- Bile contains waste materials like bilirubin, a pigment formed from the breakdown of red blood cells
- These wastes are eliminated from the body through feces, giving it its characteristic color
4. Neutralization of Stomach Acid
- Bile is alkaline and helps neutralize the acidic chyme entering the duodenum from the stomach
- This creates a suitable pH for digestive enzymes in the small intestine
What Are Common Liver Diseases?
Liver diseases are conditions that impair the liver's structure or function, affecting its ability to digest nutrients, detoxify harmful substances, and regulate metabolism. These diseases can range from mild, reversible inflammation to serious, life-threatening conditions like liver failure or cancer. Liver diseases may result from viruses, toxins, alcohol, fat accumulation, genetic disorders, or autoimmune reactions.
1. Hepatitis
- Inflammation of the liver, often caused by viral infection (Hepatitis A, B, C, D, E)
- Can also be due to alcohol, drugs, or autoimmune diseases
- Symptoms: fatigue, jaundice (yellowing of skin/eyes), dark urine, abdominal pain
- Chronic hepatitis can lead to liver damage or cirrhosis
2. Fatty Liver Disease (Hepatic Steatosis)
- Fat buildup in liver cells not caused by alcohol (NAFLD) or due to alcohol use (AFLD)
- Often linked to obesity, diabetes, and high cholesterol
- May progress to non-alcoholic steatohepatitis (NASH), cirrhosis, or liver cancer
3. Cirrhosis
- Late-stage liver disease marked by permanent scarring (fibrosis)
- Caused by long-term damage from hepatitis, alcohol abuse, or fatty liver disease
- Symptoms: easy bruising, fluid buildup, confusion, enlarged abdomen
- Can lead to liver failure or liver cancer
4. Liver Cancer
- Most common type: Hepatocellular carcinoma (HCC)
- Often develops in people with cirrhosis or chronic hepatitis B/C
- Symptoms: weight loss, upper abdominal pain, jaundice, fatigue
- Early detection improves treatment outcomes
5. Hemochromatosis
- A genetic disorder causing excess iron absorption
- Excess iron builds up in organs, especially the liver
- Can lead to cirrhosis, heart problems, and diabetes
6. Wilson's Disease
- Rare inherited disorder causing copper accumulation in the liver and brain
- Symptoms include jaundice, behavioral changes, and movement disorders
- Requires lifelong treatment to prevent liver and neurological damage
7. Autoimmune Hepatitis
- Immune system attacks healthy liver cells, causing chronic inflammation
- Can lead to cirrhosis if untreated
- Treated with immunosuppressive medications
8. Primary Biliary Cholangitis (PBC)
- Chronic autoimmune disease that slowly destroys bile ducts in the liver
- Leads to bile buildup, liver damage, and cirrhosis
- Symptoms: fatigue, itching, dry eyes/mouth
9. Liver Failure
- Occurs when the liver loses its ability to function
- Can be acute (sudden) or chronic (progressive)
- Requires urgent medical treatment, sometimes a liver transplant
How Can We Maintain Good Liver Health?
Maintaining good liver health is essential for supporting the body's digestion, metabolism, detoxification, and overall balance. The liver is a vital organ that can regenerate and repair itself, but prolonged stress from poor lifestyle choices, infections, or toxins can lead to irreversible damage. Protecting your liver involves healthy habits, regular screenings, and avoiding harmful exposures.
1. Eat a Balanced, Liver-Friendly Diet
- Focus on whole grains, fresh fruits, vegetables, lean proteins, and healthy fats
- Include antioxidant-rich foods (like berries, leafy greens, turmeric) to combat liver inflammation
- Limit saturated fats, refined sugars, and processed foods, which contribute to fatty liver disease
- Stay hydrated with plenty of water
2. Maintain a Healthy Weight
- Obesity increases the risk of non-alcoholic fatty liver disease (NAFLD)
- Combine a nutritious diet with regular exercise to reduce liver fat and inflammation
3. Exercise Regularly
- Engage in at least 150 minutes of moderate physical activity per week
- Helps lower cholesterol, improve insulin sensitivity, and reduce fat accumulation in the liver
4. Limit Alcohol Intake
- Excessive alcohol is a major cause of liver inflammation and cirrhosis
- Follow recommended limits: no more than 1 drink/day for women, 2 drinks/day for men
- Avoid binge drinking altogether
5. Avoid Unnecessary Medications and Toxins
- Overuse of drugs like acetaminophen (paracetamol) can damage liver cells
- Avoid exposure to chemical toxins, including pesticides and industrial solvents
- Always follow dosage instructions and avoid mixing medications with alcohol
6. Get Vaccinated
- Vaccines for hepatitis A and B can prevent virus-related liver diseases
- Practice safe hygiene and avoid contaminated food and water in high-risk regions
7. Avoid Illegal Drugs and Sharing Needles
- Intravenous drug use is a major risk factor for hepatitis B and C, which can lead to chronic liver damage
- Never share needles or personal hygiene tools like razors or toothbrushes
8. Don't Smoke
- Smoking introduces toxins that burden the liver and increase the risk of liver cancer
- Quitting tobacco reduces liver stress and enhances detoxification efficiency
9. Manage Chronic Conditions
- Control diabetes, high blood pressure, and high cholesterol, as these conditions increase liver disease risk
- Take prescribed medications under medical supervision and attend regular checkups
10. Schedule Regular Liver Function Tests
- Blood tests like ALT, AST, ALP, and bilirubin levels can detect early signs of liver damage
- Especially important if you have risk factors like alcohol use, obesity, or viral hepatitis
Take These Quizzes
Conclusion
In this liver lesson, we've learned about the liver, understanding its complex structure, vital functions, and the common diseases that can compromise its health. We've learned that the liver is a vital organ that is a sophisticated system responsible for detoxification, bile production, and metabolism, working tirelessly to keep our bodies in balance. Understanding the liver's anatomy and the diseases that can affect it highlights the importance of proactive liver health management.
Rate this lesson:
 Back to top
Back to top


(84).jpg)

